Prescription Drug Monitoring Programs (PDMPs) are state-wide databases used to track, analyze and report information about prescription pharmaceuticals. While PDMPs have been around in some form since California established the first continuous program in 1939, the advent of electronic data collection, storage and potential sharing catapulted PDMPs into wider use at the start of the 21st century.
In 2003, the United States Congress established the Harold Rogers PDMP competitive grants, which are issued to states by the Bureau of Justice Assistance. Only a handful of states had established PDMPs when the program was initiated.
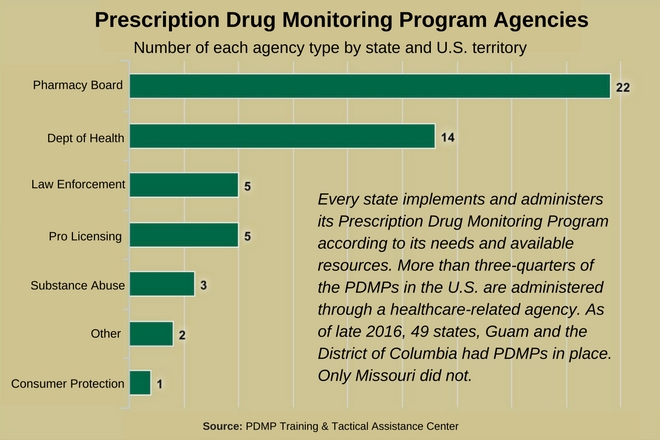
As of late 2016, 49 states and Guam had operational PDMPs, and the District of Columbia had initial PDMP infrastructure in place. The exception was Missouri, where a PDMP bill was defeated in the state legislature (St. Louis County does have a local PDPM database).
PDMP Goals
The specific goals of PDMPs vary from state to state, but usually include:
- Preventing patients with multiple prescriptions from using non-compatible drugs (polypharmacy)
- Preventing over-prescription and fraudulent dispensing of controlled substances
- Curbing the non-medical abuse of prescription drugs, particularly Schedule II narcotics such as morphine, oxycodone and methadone
- Reducing instances of diversion (channeling of drugs for illegal use)
- Facilitating the sharing of prescription information electronically around the state and nationwide
- Providing crucial prescription drug distribution and diversion data for law enforcement agencies, state health departments and other agencies.
On the federal level, the U.S. Department of Justice and the Office of National Drug Control Policy both have endorsed PDMPs as a tool to fight a proliferation of opioid abuse. This emphasis on PDMPs was a response, in part, to recent data from the Department of Health and Human Services that revealed 3.8 million Americans age 12 and older were misusing prescription pain relievers.
The sense of urgency was fueled by the fact that more than 60 percent of the 47,000 drug overdose deaths in the U.S. in 2014 involved opioids.
U.S. Attorney General Loretta Lynch issued a strategy memo in the fall of 2016 that emphasized the role of PDMPs as part of the federal government’s drug-abuse prevention plan. Strengthening PDMPs nationwide is a key component of the plan, and it was given a monetary boost by an $8.8-million grant to 20 states to help “create, implement and enhance PDMPs.”
The implementation and enhancement of PDMPs around the country also was endorsed by the National Association of State Controlled Substance Authorities (NASCSA) in an October 2016 resolution. In it, the NASCSA applauded the nationwide use of PDMPs to monitor all controlled substances in Schedules II-V.
Who Benefits from PDMPs?
The main beneficiaries of a functional PDMP are the consumers who rely on prescription drugs to treat chronic pain and other maladies. Pharmacists, physicians, nurse practitioners and others responsible for filling and/or issuing prescriptions can use a PDMP to ensure:
- Safer drug prescribing for patients
- A reduction in overprescribing and fraudulent prescribing
- Reduced risks related to potentially harmful drug interactions (polypharmacy).
In states where law enforcement agencies can access the PDMP, officers and data analysts with those agencies can use the information to track and prevent diversion, or the distribution of controlled substances for illegal purposes.
Regulatory agencies such as state departments of health can use data from PDMPs to improve the depth of knowledge about opiate misuse, abuse and overdose. Improved knowledge can help officials establish effective preventive measures and, in theory, reduce the number of overdose deaths in the U.S.
A study released on the Health Affairs website in June 2016 concluded that PDMPs prevent one opioid-related death every two hours in the U.S. The study also said that the more robust a state’s PDMP program, the more effective it is at saving lives.
Potential PDMP Shortcomings
The states and territories that establish PDMP databases do so through different agencies, based on the specific needs in the state and the availability of resources. Three-quarters of the existing PDMPs are operated by health-related agencies. Others are run by agencies related to law enforcement, professional licensing or consumer protection.
The Harold Rogers PDMP grants have helped to accelerate the implementation of PDMPs around the country, and the Centers for Disease Control and Prevention recently announced that it would award $18 million over a three-year period to 13 states and the District of Columbia in an effort to reduce opioid overdoses.
During the 2016 fiscal year, the CDC dedicated more than $50 million in investments with state health departments to underwrite PDMPs and help combat drug overdose.
Yet proponents of PDMPs still must contend with a number of potential shortcomings. These include:
- Inconsistent time frames for data sharing – some programs provide prescription information in hours, others require weeks
- Potential “chilling” effect on physicians who fear legal retribution under increased scrutiny
- Patient concerns about privacy
- Concern about harming the patient-physician relationship, which relies on trust
- Increase in use of illegal drugs (heroin, etc.) that are not tracked on the PDMP database.
Despite these concerns, PDMPs have become one of the most valuable tools available to healthcare providers, law enforcement officers and regulatory agencies in the ongoing attempt to curb opiate misuse and abuse. Rapidly improving methods for the electronic sharing of health records also will contribute to the continued expansion of PDMPs, with the goal of implementing real-time data sharing as soon as possible.
One more thing that bears watching: The U.S. Senate could soon debate whether nationwide use of PDMPs should become the law of the land. A bill was introduced in July 2016 that would require the use of PDMPs when painkillers are prescribed.