In 2015, the Office of the National Coordinator (ONC) for Health Information Technology laid out its plan for achieving interoperability, the Shared Nationwide Interoperability Roadmap. Since then, the office has been working to make interoperable health systems a reality.
The ONC is housed within the U.S. Department of Health and Human Services and is charged with “nationwide efforts to implement and use the most advanced health information technology and electronic exchange of health information,” according to healthit.gov.
And there has been significant progress on creating an interoperable framework that allows for health systems and providers to connect their data sources and speak to each other in meaningful ways, but communicating that to the public can be tough at times.

Healthcare information is, by nature, complex, more so than banking information, a popular parallel for how interoperability should work.
“People like to use the ATM analogy of ‘I can go to any ATM I want and I can get my money.’ But I would remind folks that is not the way it always was,” says Morris. “There was a time you couldn’t go to any ATM, you had to go to your bank and it took the banking industry time to work through that. Health information is inherently more complex than numbers in your bank account. We’re not even talking about genetics mapping, just first level health information.”
Standardizing health data so that it can be understood by someone on the receiving end is an intricate process that takes a great deal of time. Compounding the difficulty of completing such a task is the sensitivity of the information.
“At the end of the day, I don’t necessarily care if you find out how much money I have in my bank account,” says Morris. “I care if you steal it, but I don’t care if you know the number. I probably do care if you know specific medical information about me, particularly if I have a specific condition, mental health or substance abuse issues. From a security perspective, we’re dealing with much more serious issues than other industries, such as banking.”
The Impact of the 21st Century Cures Act
The ONC’s work in 2017 has been significant, fueled by the funding and power handed to the ONC by Congress as part of the 21st Century Cures Act. The legislation called for innovation that would help facilitate full network-to-network exchange of health information and it put the onus on the ONC to help drive those efforts.
Cures includes specific goals that play into the direction the roadmap wants to go, such as the development of a Trusted Exchange Framework. The ONC has been hard at work developing a draft version of the Trusted Exchange Framework and Common Agreement.
Currently, many health information networks exist, but they do not actually communicate with one another. Some may be regional, others take a national focus. To achieve interoperability, the systems must communicate and participate in a trusted exchange of health information. The framework is meant to act as that bridge between these entities.
“Sometimes the reason health information networks don’t talk to each other is technological, maybe it’s a difference in data formats or technical standards,” says Morris. “But for the most part, it’s business practices, terms and conditions and policy and procedures that vary across them.”
Morris points to identity proofing and authentication as a prime example. One network may require proof of identity at a basic level, Facebook for example, but for others it’s a higher bar, that may require in-person verification providing identification, maybe even biometrics.
“When you have those kind of inconsistencies, those two networks aren’t going to talk to each other,” says Morris. “Because the network with the higher security requirement isn’t going to trust the one with a lower security requirement.”
The 2015 roadmap laid out reasonably clear goals and, as 2018 represents a year of new challenges, the work the office did in 2017 and the changing healthcare landscape has set the stage for some big developments in interoperability.
The Roadmap
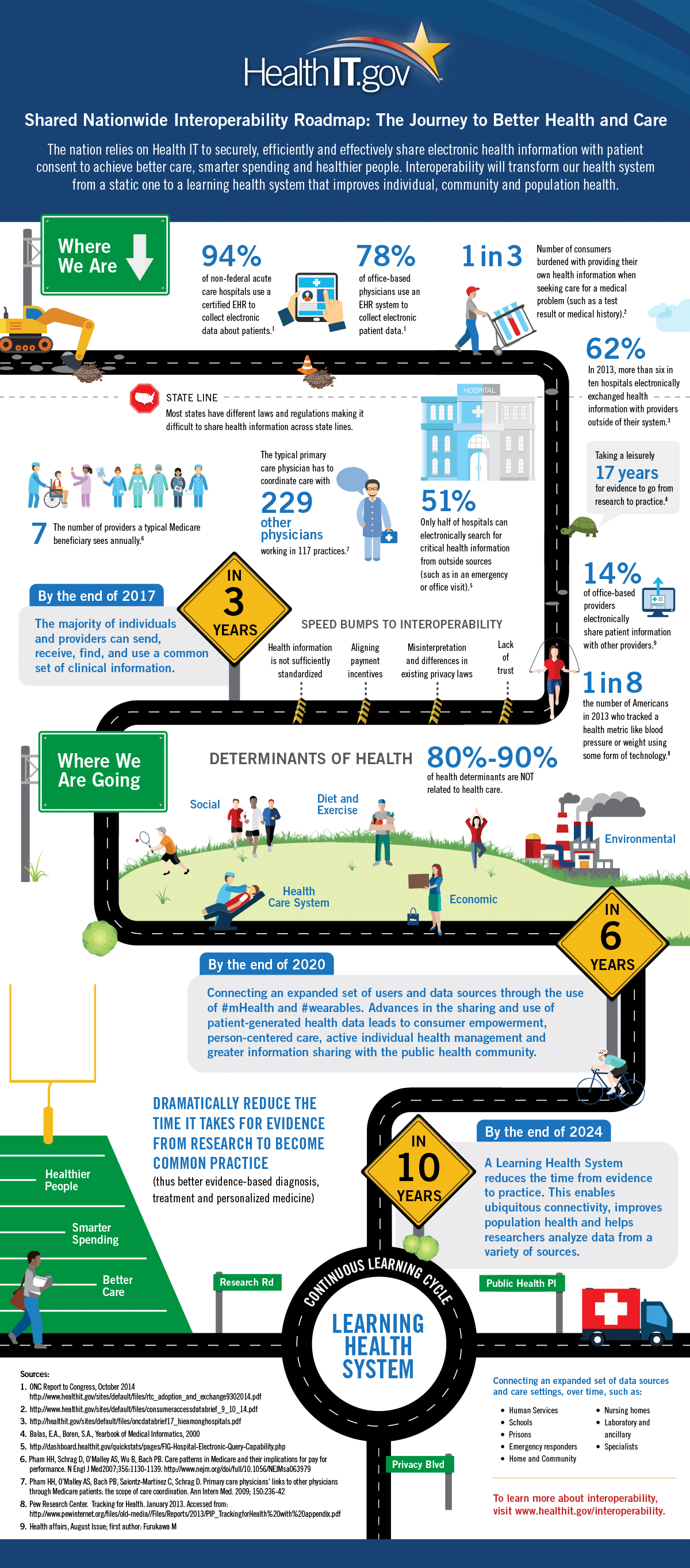
You may have seen the following infographic floating around the web at some point over the last few years. It depicts the ONC’s roadmap for interoperability.
The graphic also lays out the goals and even highlights impediments, one of which is a lack of trust between providers. The draft version of a Trusted Exchange Framework is a vital component to creating that trust.
“Congress asked us to step in and work with the industry to understand the differences in those networks and work with them to address those issues,” says Morris. “We’ve held three public listening sessions, a public comment period and are talking to stakeholders and our partners, such as the Department of Veterans Affairs, Social Security Administration and Department of Defense (DOD), to determine what we should be focusing on and make sure we understand what our partners’ needs and struggles are. We’ll be releasing a draft of the trusted exchange framework and opening it up for public comment and then we’ll move it to the next phase next year.”
One of the goals the roadmap set was to have systems in place that allow the majority of people and providers to send, receive, find and use a common set of clinical information. While the goal has not been entirely achieved, progress has been significant according to Morris, who highlighted an increase from 94% to 96% adoption of certified EHRs among hospitals, according to internal 2015 data. The increase for office space physicians (ambulatory doctors) was even more significant, jumping from 78% to 87%.
As far as providers actively exchanging data, the office has seen a significant increase in activity. From 2013-15, the percentage of hospitals exchanging information went from 62% to 82%, while office space providers went from 14% to 48%.
But perhaps just as important is the level of patient engagement.
“We’ve also seen an increase in patients accessing their data. Now, four-in-10 individuals have access to their medical data,” says Morris. “I use my provider’s patient portal all the time to message my provider and look at physician notes. Five years ago, that wasn’t something I could do.”
Coming up in part 2 of The State of the Shared Nationwide Interoperability Roadmap, Morris discusses the challenge of battling information blocking, incorporating wearables into the spectrum of care and more.