The advent of big data over the course of the past decade has had a profound effect on healthcare in the United States. Advances in computer science and digital communication continue to transform the way health information is collected, shared, stored and used to help improve prevention and treatment methods.
Big data in healthcare constitutes the large volume of information generated by communication and other interaction among patients, physicians, hospitals, medical clinics, healthcare administrators, insurance companies, pharmaceutical companies, government agencies and other stakeholders.
In addition to the adoption of technological advances in medical offices and clinics, a number of federal laws related to electronic healthcare data gave the industry a push toward digitization.
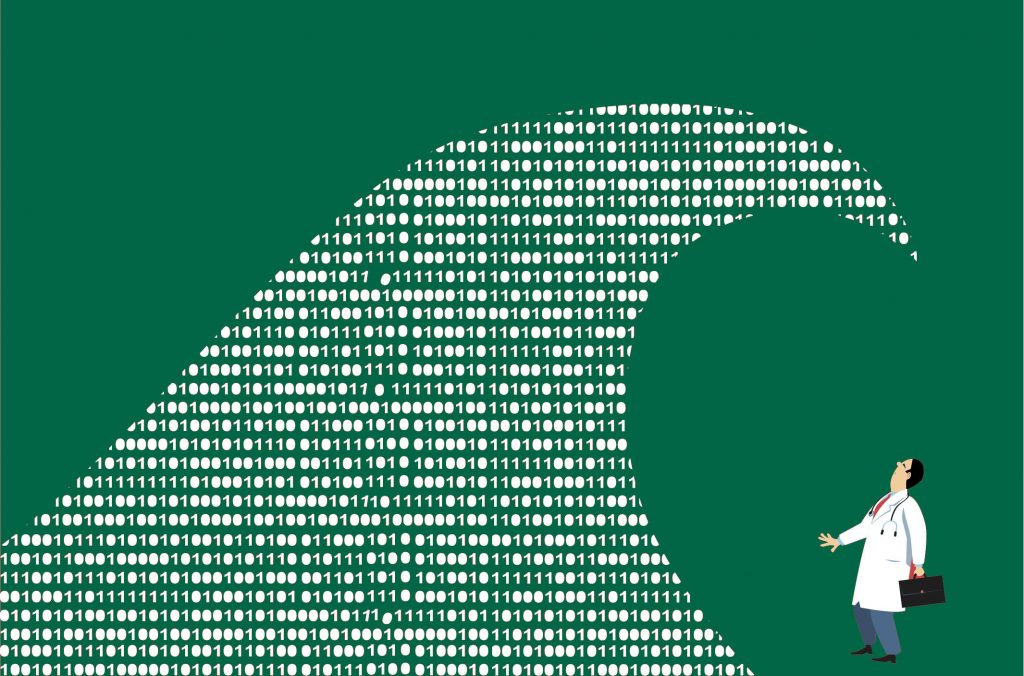
How quickly has the pool of healthcare data grown? Since the implementation of the Health Data Initiative by the U.S. Department of Health & Human Services in 2010, the public website HealthData.gov has expanded from 10 datasets at its inception to more than 3,000 datasets at the start of 2017. Physicians, healthcare administrators and other stakeholders no longer can be expected to master the volume of information associated with their areas of expertise.
The rapid expansion of available healthcare-related data created the need for innovative ways to store, organize and analyze the medical information used to improve the efficiency of healthcare delivery.
In addition, a shift in the way Medicare and Medicaid reimbursements are determined created the need for more accurate and reliable healthcare data. Whereas payments used to be determined on a fee-for-service basis, in the wake of the HITECH Act of 2009, the Centers for Medicare & Medicaid Services (CMS) established payment based on “meaningful use,” or treatment outcomes.
This major shift meant physicians and the CMS required a much deeper, richer set of data in order to assure timely and fair reimbursements.
Meaningful use is one of many drivers of big data in healthcare. Here are other ways the emergence of Big Data is shaping the U.S. healthcare system:
- An increased importance in cybersecurity. More online data means greater vulnerability to cyber attacks, including malware, spyware and ransomware. In 2015, the U.S. Congress mandated a heightened level of security to protect the preponderance of health data. HIPAA laws governing the protection of personal medical information are a major consideration when it comes to security.
- The rise of major big data vendors in healthcare. Corporations grounded in information technology and data analysis saw a demand from hospitals and other health providers for services that incorporate more efficient data gathering methods and more secure data storage. With decades of research and development behind them, large technology companies are suited to the demands of the healthcare industry and are driving innovation in interoperability, as well as digital connectivity of medical devices.
- An increased emphasis on healthcare value. With meaningful use and other major changes in the U.S. healthcare system, consumers and care providers are more focused than ever on medical costs as they relate to outcomes. Patients have come to expect that hospitals and primary care facilities use the most up-to-date methods to gather and share information. For example, many physicians have significantly reduced the use of paper prescriptions in favor of transmitting the order directly by computer to a pharmacy. The more efficient a doctor’s office is, the more confidence a patient will have that he or she is receiving the best possible care, and Big Data implementation is an important path to greater efficiency.
- Communication is becoming more efficient at reducing fraud, waste and abuse. Directly tied to the practice of transmitting prescriptions by computer is the increased prominence of Prescription Drug Monitoring Programs (PDMP), which are state-maintained databases that provide physicians and pharmacists information about a patient’s drug use. Without a PDMP or similar database, a pharmacist essentially is operating in the dark when it comes to a patient’s background with a particular prescription medication. The use of Big Data enables physicians, pharmacies and law enforcement to stay on the same page when it comes to curbing the abuse of prescription medicine.
One big question about big data and healthcare is this: Can analytic capability keep up with the preponderance of data? The answer is maybe.
The U.S. Bureau of Labor Statistics (BLS) estimates that the number of jobs related to gathering, storing, analyzing and sharing health-related data will grow by 15% through 2024. That’s twice as fast the growth rate for all job types, but it doesn’t necessarily mean that labor supply will meet the demand for competent healthcare data analysts.
What it does mean, however, is that in all likelihood, demand will continue to be strong in the foreseeable future for professionals with experience in big data and healthcare, and the academic credentials to back up that experience.